It's that time yet again, ladies and gentleman. Time once again to say goodbye to the raging shitmaelstrom that was 2017, and hello to the brand new year. 2018! The year where everything will suddenly be so much better! This will be the year frauds and mountebanks will cower under the supreme reign of science and evidence, and when incompetent orange quarterwits will no longer be in charge!
Ha. Ha. No. We all know that won't fucking happen. But instead of wallowing in pseudoscientific misery, let's instead (as promised) enjoy this rousing interview with my wife, Mrs. Bastard (not her real name™).
You asked the questions, and she's graciously answered them. Questions I've deemed too personal have been unreservedly ignored and/or sent to live in the White House with Mr. Trump, because censorship is totally fucking legal (and in fact actively encouraged) in Bastardia. So without further ado, I give you my wife.
Please.
Ha haha ha. Siiiigh.
What's DocBastard's embarrassing secret/s? (from Timethyfx)
I don't know. *turns to me* Do you have any? {No. Of fucking course not. I air all my dirty laundry right here.}
What is your favorite blog post? (from Casi G)
I guess I would have to have read them to be able to answer that. No, actually Doc tells me all of the stories the second he gets back from the hospital, no matter if I'm enjoying my morning coffee or taking a shower or whatever. I get to relive them all personally and in all their gory detail.
What is your favorite holiday and why? (from Angel)
My favourite time of year is December, as the general population tends to be kinder, more understanding, more patient, and more at peace with each other.
What is Doc's "tell" that there is a new story forming? (from Ken Brown)
Usually when he gets home, sighs, smiles, and says, "You're not going to believe this one". And then I respond by saying, "That sounds like a blog post!"
How stressed is Doc at home about work? (anon)
He's most stressed when he's lost a patient that he feels he shouldn't have, or if he has a patient who's very sick and he can't figure out why.
What brings tough ole Doc Bastard to tears? (from Nautipirate).
I can't think of anything that's brought him to tears. {You're goddamned right there isn't.} Perhaps a spoiled beer. {Nope.} The last piece of lasagne? {Nah.} The end of season 7 of Game of Thrones with a year and a half to wait until season 8? {Ok, you got me there. *sniff* Dammit, I got something in my eye.}
How is grocery shopping with the DocBastard? (from Cali)
Do we grocery shop together? Have we ever been grocery shopping together? {For the record - YES WE HAVE. God damn it.}
Would you want your kids to be Doc Bastard juniors? (from Joan B)
Aren't they already DocBastard juniors? But if you're asking if I want them to be doctors, no. NO. NO NO NO NO NO NO.
In other words, no.
Is Doc any good at carving the turkey? (from tania cadogan)
What do you think? Does a bear shit in the woods?
Whats the best thing Doc can cook? (from Shark)
He makes a mean fresh fettuccini with bolognese.
We know what doc thinks of shows like House, but what does Mrs. Bastard think? (from Connor)
I think they're largely entertaining, as long as you buy into willful suspension of disbelief. {And can put up with me constantly yelling at the television because they've royally fucked something else up AGAIN. Come on, Hollywood. I'm available for consulting work. Call me.}
How did you come to marry Doc? Did he propose on bended knee, did you propose to him, or did you just both decide it was time? (from Cleopatra)
He proposed on bended knee. I feel like he should have been on both knees. And he also should have chosen a location that we could go back and visit that wasn't destroyed. {No, I'm NOT TELLING, so don't even ask.}
How long have you two been married? (From Not your average housewife)
Long enough. {Love you too, dear.} No, it seems like just yesterday. Long enough to put up with each others' idiosyncrasies and even be fond of some of them. Long enough to finish each others' sentences and know what each other is thinking, but not long enough not to discover new things about each other. {Aww, no seriously, I love you too, dear.}
What's the best present Doc ever gave you? (Excluding your perfect offspring, of course.) (from RC)
My cappuccino machine. And that big green sweater with the giant gold buttons that was probably the most hideous thing I've ever seen. {Really? Come on, I barely knew you then. Are you ever going to let that go?)
How do you keep your household running smoothly? Does Doc help with the dishes? (anon)
WD40. It keeps everything running smoothly. No, lists, lists, and more lists. Speaking of lists, have you changed that light bulb over the piano yet? It's been TWO YEARS. {No, because it's only been 2 years.} And did you empty the dishwasher? {Yes.}
What made you fall in love with Doc, and he with you? (anon)
I think there was instant attraction and chemistry, but I don't know what made me fall in love with him. It must have been his charming personality and his wit. {I swear I didn't make that up. Those were her exact words. Honest.} It certainly wasn't his taste in clothes. Or hideous green sweaters with giant gold buttons. {Oh, har dee fucking har har.}
Do you have any advice for newly weds/ new parents/just random pieces of good general life advice? (from the small raven)
Advice for newlyweds: 1) Don't marry a trauma surgeon. 2) Never go to bed mad at each other. 3) Respect each other.
Advice for new parents: 1) Don't throw the baby against the wall. 2) Don't throw the baby against the wall. 3) I mean it, don't throw the baby against the wall. 4) Don't worry, projectile vomit and pee do come out in the laundry and don't leave a stain. Usually.
Random good life advice: Be good, and do good. {See why I married her?}
What is Doc's favorite dish for you to cook and will you share the recipe? (from Promise)
His favourite thing is lasagne. I use the Fanny Farmer recipe. Google it. {She doesn't like to share recipes for some reason. Don't Google it - I've done it for you. Just click the first picture.}
We all know that Doc Bastard has a fascination for pulling various things out of rectums. What is the best "removed from rectum" story he's ever told you? I bet it wasn't the one he told US! (from Wednesday)
Actually, it is. It's the Coke bottle story, for sure. I think that's one of his first blog posts. And it was his first RFO. Still the best. That was a great story. {Yes, yes it was.}
If DocB were an animal (of the non-human sort) what animal would he be? What would you be? What kind of hybrids would the Little Bastards be? (anon)
He would be a non-lazy animal. He would be an industrious, cute animal. I think he would be a beaver, because he can whittle things out of wood. I, on the other hand, would be a honey badger. Why? Because honey badger doesn't give a shit. Our hybrid son would be a sloth-hyena because he likes to hang off things and makes way too much noise all the time. Our hybrid daughter would be a unicorn. {Because why the hell not.}
Does Doc utilize any of his surgical skills at home? Can he sew a hem? (from OldFoolRN)
He uses his surgical skills all the time at home. Let's put it this way - when a hem needs to be sewn or a button needs to be replaced, it's not Mrs. Bastard doing it. I just say, "Daddy Bastard, can you please sew this for me or close this hole in this stuffed animal or replace its arm?" I can also guarantee the button will never fall off again. {For the record, MomBastard taught me to sew when I was about 8, though I do usually use surgical knots which she did not teach me.}
If you could magically change Doc's profession, what would you have it be? What type of place would be your dream retirement destination? (from Hippodamia)
I would change his profession to personal chef. Because then I would never have to cook again. {What, you think I'd still bring my work home with me?} And he would have better hours. Our dream retirement destination would be someplace where it's 28 degrees {that's Celcius} all year round, people are nice, life isn't so rushed, but has access to all the amenities and culture of a big city. {That place doesn't exist, dear.}
What kind of movies do you like and what do you watch together? (from Scott Aylor)
I like comedies. {I like sci fi}. I can't remember the last time we watched a movie together and didn't fall asleep. Am I asleep right now? Are we still doing this interview right now?
---
There you have it, folks. Another year and another interview wrapped up. I'll see if Mrs. Bastard is up for another interview next year. If she hasn't killed me yet. Maybe I'll have even changed the light bulb over the piano by then.
Probably not.
Happy New Year!
Stories about general surgery, trauma surgery, dumb patients, dumb doctors, and dumb shit from the dumb world around us.
Sunday, 31 December 2017
Monday, 18 December 2017
Branding
Oh, boy. We have a bit of a doozy here. As you all know this blog is mainly about stupid people doing stupid things. Sometimes, however, it is about smart people doing stupid things (namely me, if I do say so myself). This is one of those times. Except that this time, the smart person gloriously isn't me at all. Have no fear, it is still about a smart person, a surgeon even, having done a very stupid thing.
Indeed this story is about Simon Bramhall, a rather famous British transplant surgeon who gained fame in 2010 by transplanting a liver that was being transported by a plane that crashed. They managed to salvage the organ and he transplanted it successfully. I think we can all agree that that is a Very Good Thing.
But in 2013 Simon did a Very Stupid Thing. He was performing a liver transplant on February 9, when for some inexplicable reason he decided to burn his initials "SB" onto the surface of the organ he was transplanting. Before you start yelling, "Oh come on, he couldn't have done that. It was probably just misinterpreted. What type of egomaniac would do that?" Bramhall would, that's who. The instrument he used was an argon beam coagulator which is designed to effect (yes, 'effect') haemostasis on the surface of a bleeding organ, and yes he branded his initials onto the liver. Keep in mind this was a very superficial injury that he inflicted, one that would be expected to heal very quickly.
If that doesn't sound too bad, have no fear, because it gets worse. He did the exact same thing 7 months later, again branding his initials on a transplanted liver. Again, anyone who understands how livers heal knows that these marks should disappear quickly and completely. Unfortunately, they did not on one of these two patients. Another surgeon re-operating on one of the patients some time later noted "SB" still visible on the surface of the liver, and Dr. Bramhall was busted.
Dr. Bramhall was suspended initially, and he resigned from the hospital the next year. Further, he was arrested and charged with both assault occasioning actual bodily harm (to which he pleaded not guilty), and assault by beating, to which he admitted and was convicted.
Wait wait, assault by beating? How is that possible?
Right, I was as confused as you at first. It seems that the prosecutor didn't know exactly how to charge him, because this past week he stated that there was just no legal precedent for this type of injury. (Seriously, what the hell would you charge him with? Arson? I have no idea. This is one of approximately 2,490 reasons why I'm not a lawyer.) Regardless, the prosecutor did state that Bramhall's admission of guilt indicates that he admits that "what he did was not just ethically wrong but criminally wrong". Sentencing is scheduled for January 2018. I suspect the judge is just as clueless about how to punish him appropriately.
Bramhall was also issued a formal warning earlier this year from the General Medical Counsel which said regarding his behaviour, "It risks bringing the profession into disrepute and it must not be repeated. Whilst this failing in itself is not so serious as to require any restriction on Mr Bramhall’s registration, it is necessary in response to issue this formal warning."
And that is where I vehemently disagree.
In my opinion Bramhall deserves to be struck off the record, to lose his licence to practice. This falls so far outside the bounds of the normal, ethical, responsible behaviour of a physician that something more drastic than a proverbial slap on the wrist is in order. Bad behaviour by surgeons used to be tolerated, and everyone would just look the other way whenever it happened. Harassing nurses, inappropriate comments, throwing instruments, yelling at students, demeaning residents, and other assorted temper tantrums were commonplace in the operating theatre until recently. Nowadays, however, these sorts of outbursts are no longer permissible. Surgeons are now reprimanded and punished for bad behaviour.
But knowingly and purposefully injuring a patient?
Inexcusable.
I have heard the counterargument that no real harm was done, so it isn't that big a deal. Really? Is that a logical argument? Then by that same logic we should just allow people to drive drunk as long as they don't injure anyone, because no harm is done. Right? Right?
No, not right. Not right at all.
However, not everyone agrees with me. In fact, when he was suspended in 2014 one of his former patients said, "Even if he did put his initials on a transplanted liver, is it really that bad? I wouldn’t have cared if he did it to me. The man saved my life." It's true though, right? The liver heals very quickly, and even if it doesn't heal completely, having a scar on the organ won't affect its function one bit. So it's not a big deal, right?
Wrong. I've written before about the trust that patients put in their doctors, but especially their surgeons. Imagine the amount of faith people must have to allow themselves to be put completely to sleep, completely vulnerable, absolutely at our mercy, and trust that we not only do our best to put them back together but do it with dignity and respect.
Dr. Bramhall violated that dignity. He violated that trust. Not just one, twice.
I don't know if it was a momentary lapse of reason (twice), sociopathy, or simply a massive ego that led Bramhall to do what he did. Yeah, I'll be the first to admit that many surgeons have massive egos (yours truly excluded, of course). But quite frankly, I don't care a whit. I couldn't give a rattus rattus' posterior, because after pondering this since the moment this story broke, I've come to the realisation that there is literally not a single legitimate excuse in the world that would permit a surgeon to brand a patient like this. Not one.
Not one.
Indeed this story is about Simon Bramhall, a rather famous British transplant surgeon who gained fame in 2010 by transplanting a liver that was being transported by a plane that crashed. They managed to salvage the organ and he transplanted it successfully. I think we can all agree that that is a Very Good Thing.
But in 2013 Simon did a Very Stupid Thing. He was performing a liver transplant on February 9, when for some inexplicable reason he decided to burn his initials "SB" onto the surface of the organ he was transplanting. Before you start yelling, "Oh come on, he couldn't have done that. It was probably just misinterpreted. What type of egomaniac would do that?" Bramhall would, that's who. The instrument he used was an argon beam coagulator which is designed to effect (yes, 'effect') haemostasis on the surface of a bleeding organ, and yes he branded his initials onto the liver. Keep in mind this was a very superficial injury that he inflicted, one that would be expected to heal very quickly.
If that doesn't sound too bad, have no fear, because it gets worse. He did the exact same thing 7 months later, again branding his initials on a transplanted liver. Again, anyone who understands how livers heal knows that these marks should disappear quickly and completely. Unfortunately, they did not on one of these two patients. Another surgeon re-operating on one of the patients some time later noted "SB" still visible on the surface of the liver, and Dr. Bramhall was busted.
Dr. Bramhall was suspended initially, and he resigned from the hospital the next year. Further, he was arrested and charged with both assault occasioning actual bodily harm (to which he pleaded not guilty), and assault by beating, to which he admitted and was convicted.
Wait wait, assault by beating? How is that possible?
Right, I was as confused as you at first. It seems that the prosecutor didn't know exactly how to charge him, because this past week he stated that there was just no legal precedent for this type of injury. (Seriously, what the hell would you charge him with? Arson? I have no idea. This is one of approximately 2,490 reasons why I'm not a lawyer.) Regardless, the prosecutor did state that Bramhall's admission of guilt indicates that he admits that "what he did was not just ethically wrong but criminally wrong". Sentencing is scheduled for January 2018. I suspect the judge is just as clueless about how to punish him appropriately.
Bramhall was also issued a formal warning earlier this year from the General Medical Counsel which said regarding his behaviour, "It risks bringing the profession into disrepute and it must not be repeated. Whilst this failing in itself is not so serious as to require any restriction on Mr Bramhall’s registration, it is necessary in response to issue this formal warning."
And that is where I vehemently disagree.
In my opinion Bramhall deserves to be struck off the record, to lose his licence to practice. This falls so far outside the bounds of the normal, ethical, responsible behaviour of a physician that something more drastic than a proverbial slap on the wrist is in order. Bad behaviour by surgeons used to be tolerated, and everyone would just look the other way whenever it happened. Harassing nurses, inappropriate comments, throwing instruments, yelling at students, demeaning residents, and other assorted temper tantrums were commonplace in the operating theatre until recently. Nowadays, however, these sorts of outbursts are no longer permissible. Surgeons are now reprimanded and punished for bad behaviour.
But knowingly and purposefully injuring a patient?
Inexcusable.
I have heard the counterargument that no real harm was done, so it isn't that big a deal. Really? Is that a logical argument? Then by that same logic we should just allow people to drive drunk as long as they don't injure anyone, because no harm is done. Right? Right?
No, not right. Not right at all.
However, not everyone agrees with me. In fact, when he was suspended in 2014 one of his former patients said, "Even if he did put his initials on a transplanted liver, is it really that bad? I wouldn’t have cared if he did it to me. The man saved my life." It's true though, right? The liver heals very quickly, and even if it doesn't heal completely, having a scar on the organ won't affect its function one bit. So it's not a big deal, right?
Wrong. I've written before about the trust that patients put in their doctors, but especially their surgeons. Imagine the amount of faith people must have to allow themselves to be put completely to sleep, completely vulnerable, absolutely at our mercy, and trust that we not only do our best to put them back together but do it with dignity and respect.
Dr. Bramhall violated that dignity. He violated that trust. Not just one, twice.
I don't know if it was a momentary lapse of reason (twice), sociopathy, or simply a massive ego that led Bramhall to do what he did. Yeah, I'll be the first to admit that many surgeons have massive egos (yours truly excluded, of course). But quite frankly, I don't care a whit. I couldn't give a rattus rattus' posterior, because after pondering this since the moment this story broke, I've come to the realisation that there is literally not a single legitimate excuse in the world that would permit a surgeon to brand a patient like this. Not one.
Not one.
Monday, 11 December 2017
Now I've heard everything
Most of the mechanisms of injury I see are rather mundane and pedestrian. Auto accidents, falls, stabbings, shootings, pedestrians struck, bicycle accidents, and assaults are the mainstays of what I see, do, and fix. Sometimes I get the "other", however. These can be anything from ordinary (dog bite) to a bit strange (chainsaw to the face) to how the hell did that happen (foot run over by a lawnmower) to what the actual fuck (bitten by a camel). To be honest, it's difficult to come up with a mechanism of injury that I haven't seen.
Until someone does.
Saturday night seems to go along with alcohol just like peas and carrots, peanut butter and jelly, salt and pepper. It just doesn't seem to flow linguistically, however. Hm. Anyway, I'm constantly astounded at what drunk people will do to themselves or others, simply because they are drunk. It doesn't seem to matter what they do or to whom they do it, as long as they can blame alcohol.
"Hi Doc, good evening. This is Dawn (not her real name™). Dawn was assaulted with bug spray tonight, and . . ."
I don't typically interrupt the medics in the middle of a patient presentation, but this time I couldn't help myself.
"Wait wait wait . . . what?"
The medic chuckled a bit and continued. "Heh, yeah. Anyway, she was assaulted with bug spray after her and her boyfriend got into a fight after a night of heavy drinking. She's got a lac on her scalp about 5 cm, positive loss of consciousness. She's 49 years old, history of HIV, not taking any meds, no allergies. Only complaining of a headache."
If you're following along here, you probably have the same question I had. I could not resist the temptation and just blurted it out:
"So, was she hit with the can or sprayed?"
"Heh. Yeah, Both."
Fortunately the spray didn't get in her eyes, so all she needed was a few staples to close the wound and a heavy dose of IV fluid to get her sober. Once she was coherent, her boyfriend came to take her home. All was forgiven, apparently.
I know I've said this several times before, but this time I really really really mean it:
NOW I've seen everything.
Until someone does.
Saturday night seems to go along with alcohol just like peas and carrots, peanut butter and jelly, salt and pepper. It just doesn't seem to flow linguistically, however. Hm. Anyway, I'm constantly astounded at what drunk people will do to themselves or others, simply because they are drunk. It doesn't seem to matter what they do or to whom they do it, as long as they can blame alcohol.
"Hi Doc, good evening. This is Dawn (not her real name™). Dawn was assaulted with bug spray tonight, and . . ."
I don't typically interrupt the medics in the middle of a patient presentation, but this time I couldn't help myself.
"Wait wait wait . . . what?"
The medic chuckled a bit and continued. "Heh, yeah. Anyway, she was assaulted with bug spray after her and her boyfriend got into a fight after a night of heavy drinking. She's got a lac on her scalp about 5 cm, positive loss of consciousness. She's 49 years old, history of HIV, not taking any meds, no allergies. Only complaining of a headache."
If you're following along here, you probably have the same question I had. I could not resist the temptation and just blurted it out:
"So, was she hit with the can or sprayed?"
"Heh. Yeah, Both."
Fortunately the spray didn't get in her eyes, so all she needed was a few staples to close the wound and a heavy dose of IV fluid to get her sober. Once she was coherent, her boyfriend came to take her home. All was forgiven, apparently.
I know I've said this several times before, but this time I really really really mean it:
NOW I've seen everything.
Monday, 4 December 2017
DNR
If you're in the States, you can rest assured that I am most assuredly NOT writing about the Department of Natural Resources. Nor am I writing about Denbury Resources, Inc (whose unfortunate symbol on the New York Stock Exchange is DNR). No, anyone remotely familiar with the medical field (or who ever watched House MD or Holby City or Grey's Anatomy or ER or St Elsewhere or M*A*S*H or Scrubs or Marcus Welby, MD [godDAMMIT there are a lot of medical dramas!]) knows that "DNR" stands for "Do Not Resuscitate". It represents the primary right of the patient - to refuse medical treatment, even in the face of impending death. Most usually it is employed by the elderly, severely infirm, or terminally ill to alert their medical care providers that they do not want any heroic measures in the event of sudden or imminent death.
There are various elements to a DNR, including orders not to intubate, not to do chest compressions, not to employ vasopressors (medication to artificially elevate blood pressure), not to give food and/or fluids, not to use dialysis, or to use comfort measures only. The exact nature of the DNR order, including any and all therapies that may or may not be used, is explicitly elucidated in a signed document that is supposed to be readily available for medical practitioners to see. That way there can be no ambiguity if an unconscious yet terminal patient is brought to the hospital. The papers are supposed to be easy to find, though sometimes they can be difficult to track down.
Sometimes, however, the DNR is, well, let's just say sometimes it is slightly more prominent:
There are various elements to a DNR, including orders not to intubate, not to do chest compressions, not to employ vasopressors (medication to artificially elevate blood pressure), not to give food and/or fluids, not to use dialysis, or to use comfort measures only. The exact nature of the DNR order, including any and all therapies that may or may not be used, is explicitly elucidated in a signed document that is supposed to be readily available for medical practitioners to see. That way there can be no ambiguity if an unconscious yet terminal patient is brought to the hospital. The papers are supposed to be easy to find, though sometimes they can be difficult to track down.
Sometimes, however, the DNR is, well, let's just say sometimes it is slightly more prominent:
According to a case report from the New England Journal of Medicine, this 70-year old gentleman was brought by paramedics to a hospital in Miami, Florida unconscious and intoxicated. He had a history of chronic obstructive pulmonary disease, atrial fibrillation, and diabetes, and he arrived without any identification or family members. When doctors disrobed him to do their examination, they found "DO NOT RESUSCITATE" tattooed quite clearly (with "NOT" even underlined) on his chest with his signature underneath.
Open and shut case, done and done, cut-and-dried, impossible to misinterpret, right? RIGHT?
If that were an easy question to answer, I wouldn't be writing this right about now, would I.
A few hours later his blood pressure dropped precipitously due to severe sepsis, and he developed a severe metabolic acidosis (his serum pH was 6.81 - I have never seen anyone with a pH less than 6.9 survive). The intensive care doctors who attended to him had a decision to make: A) honour the tattoo as a legally binding DNR or B) treat him as they would any other anonymous patient.
They chose B.
According to lead author Gregory Holt, MD, the doctors chose to invoke "the principle of not choosing an irreversible path when faced with uncertainty", so they categorically ignored the tattoo, starting him on antibiotics, putting him on BiPAP, and starting vasopressors. In other words, everything short of intubating him.
My first reaction to this story was "WHAT? WHAT THE FUCK WERE THEY THINKING? HIS CHEST SAYS DEE EN ARE!" My next thought was that if they had done chest compressions, they would have been committing assault on this gentleman. My next thought was . . . calm the fuck down and get some more information, dumbass.
*deep breath*
It turns out cases like this, while extraordinarily rare, are not entirely isolated. In fact there is a published case report in the literature of a man with a similar "DNR" tattoo (though it is admittedly not quite as explicit) which did not reflect his actual wishes. That patient had lost a bet while drunk many years before, the loser being required to get a tattoo of "DNR" on his chest.
"Heh, sounds like one of your patients, Doc."
Indeed it does. Regardless, Dr. Holt and his team obtained a consultation from their ethics team, who determined that the tattoo most likely did reflect the patient's wishes. They advised the doctors to honour it as an ordinary paper DNR. Out of respect for the patient's (hopefully) wishes, an actual DNR order was written. Fortunately shortly thereafter the gentleman's real out-of-hospital DNR was obtained, and he passed the following morning without incident.
After contemplating this case for some time, I've come to the realisation that it isn't nearly so clear cut as I had originally thought. If I got a dying trauma patient who had a prominent and unmistakable DNR tattoo, would I really be able to say "Wait, stop, don't do anything. Look, it says DEE EN ARE right there on his chest!"? Would that really be the right thing to do without verifying it first? The part of me that explicitly respects patients' wishes says an very emphatic "Yes", but the entire rest of me (which is admittedly rather small) says "Not so fast".
I believe that treating a patient who does not want to be treated is malpractice. However, I also believe I would be obligated to verify the DNR prior to withdrawing or withholding care while consulting my own ethics team. I also also believe doing anything short of this would be malpractice.
What do you believe?
Friday, 1 December 2017
Interview part 2
Those of you who have been here a while probably (hopefully) remember the interview with Mrs. Bastard from December 2015. If you don't remember it, well, look it up. I can't do everything for you. Anyway, she just shockingly mentioned that she would like to do another one, and since I had intended that to be an annual thing, I should probably keep my word or something.
So you people are officially on duty. Submit your questions in the comments below for my dear wife, and I will choose the best and/or least revealing ones for Interview 2.0, which should be published some time next month as long as the Call Gods allow it. There are no official rules on what questions you may ask, but you'd better god damn well believe that I will categorically ignore any question I deem inappropriate or too personal. I will not be revealing my name, age, location, childhood nickname, or my most ticklish spot (upper back).
Damn it.
Everyone ready? And . . . GO.
So you people are officially on duty. Submit your questions in the comments below for my dear wife, and I will choose the best and/or least revealing ones for Interview 2.0, which should be published some time next month as long as the Call Gods allow it. There are no official rules on what questions you may ask, but you'd better god damn well believe that I will categorically ignore any question I deem inappropriate or too personal. I will not be revealing my name, age, location, childhood nickname, or my most ticklish spot (upper back).
Damn it.
Everyone ready? And . . . GO.
Monday, 27 November 2017
No story
It's been two weeks since my last update. I had a new post all edited, shined up, and ready to go, but then the patient (who had done something fully deserving to have a story written about him) decided to go and do something even stupider and have himself a postoperative complication.
No, it isn't my complication. It was an orthopaedic surgery with an orthopaedic complication, but regardless he isn't doing well. At all. So out of respect for him, I have decided to postpone his story and possibly even delete it, depending on his outcome.
If you can't tell, I'm not happy about this. Even though it wasn't my surgery and isn't my complication, he's still my patient.
Not happy.
UPDATE:
He died. The story will be deleted. God damn it.
No, it isn't my complication. It was an orthopaedic surgery with an orthopaedic complication, but regardless he isn't doing well. At all. So out of respect for him, I have decided to postpone his story and possibly even delete it, depending on his outcome.
If you can't tell, I'm not happy about this. Even though it wasn't my surgery and isn't my complication, he's still my patient.
Not happy.
UPDATE:
He died. The story will be deleted. God damn it.
Monday, 13 November 2017
Electricity
There are few things on this oblate spheroid we call Earth of which I am truly terrified. On the top of my list are nuclear annihilation (which seems more likely with the recent escalation of the Kim-Trump 12-year-old child feud), earthquakes, supervolcano eruptions, and pretty much any reptile, sea life, or insect in Australia (seriously Australia, what the fuck is up with Sydney funnel-web spiders and Irukandji jellyfish?). But a very close fifth is, as you've probably guessed from the title, electricity.
Despite excellent marks in science classes in school, I still don't fully understand electricity, nor do I really care to. I zapped the shit out of myself trying to change out a faulty light switch back in college, and since then I try to pretend electricity doesn't really exist (not really). Even static electricity shooting out of my fingertips every winter has me firmly believing that the world is constantly trying to electrocute me. My relationship with electricity now solely involves me plugging things carefully into outlets and then turning those things on and off. And as much as I enjoy fixing things, if those things involve wiring or rewiring or anything involving a fuse box, I leave it to the professionals. Because fuck electricity.
Fortunately professional electricians exist. I don't know if these people understand electricity completely, trust it implicitly, or just don't give a shit about the occasional zap that could potentially stop their heart from beating (which, though I am not a cardiologist I understand to be a Very Bad Thing). Irrespective of how or why they do it, they seem more than happy to fiddle with whatever potentially lethal electrical thing has gone awry. Unfortunately, however, not all professional electricians know what the hell they are doing.
"Electrocution" is a portmanteau of "electricity" and "execution" originally coined in the late 19th century to describe death by the electric chair. It has since come to mean any death from electrical shock (as opposed to cardiogenic shock, hypovolemic shock, and "OMG can you believe she's wearing that to a funeral??" shock). Electrical injuries are particularly difficult to treat because they often combine cutaneous thermal injuries (ie burns), internal thermal injuries (including muscle necrosis), cardiac electrical dysrhythmias, and mechanical trauma from the inevitable fall after the shock. Thankfully they are also relatively rare, and most are treated at dedicated burn facilities, which mine is not. Despite this, I still see the occasional electrical injury victim.
Like Lou (not his real name™), who was my patient, and his partner, who was not. Don't worry, I'll explain.
Lou was driving to a job when he heard over his business radio that his partner had suffered a moderate shock while repairing an air conditioning unit in an attic space. Wanting to make sure his buddy was ok, Lou diverted to that establishment, where he found his partner somewhat dazed but relatively unscathed. Apparently his partner hadn't turned off the main power before starting, and at some point he had come into contact with a live wire that was hanging from the ceiling.
Now common sense would dictate either A) your partner turning off the power prior to starting, or B) turning off the power after your partner gets a nasty shock. As you can easily tell, either way the power gets turned off. Right? RIGHT?
Common sense, I am sad to report, is no longer common.
Lou apparently decided to finish the job his partner had started without addressing the live wire hanging from the ceiling that had nearly finished off his partner. He climbed the ladder to the attic space, reached down to get a tool, and as he stood up he caught the live wire with his forehead.
Hilarity did not ensue.
The shock Lou received was significantly greater than his partner's. He was predictably thrown backwards down the ladder where various parts of his anatomy bounced off several steps, ultimately striking his head on the floor below and losing consciousness.
And that is where we pick up his story.
Lou had just started regaining consciousness when he arrived in my trauma bay. He was clearly dazed and confused, a dark electrical burn on his forehead, dried blood matting a good portion of his hair. Surprisingly his main complaint was his right shoulder. A thorough workup demonstrated a fractured clavicle, a scalp laceration, a relatively severe concussion, and a small burn on his forehead (obviously). He had no evidence of a cardiac or skeletal muscle electrical injury, but I watched him overnight just to be sure. He felt much better, though thoroughly ashamed, the next morning when I sent him home.
I get a bit miffed when doctors in other specialties suggest how I do my job, but I admittedly get a rather severe eye twitch when non-doctors do it. Despite this, before Lou left the hospital I felt entirely comfortable reminding him to turn off the goddamned electricity before working on it.
I also made sure to note which company he works for and made a mental note never to hire them. Any professionals working on my power lines need to know what the hell they are doing and, you know, not die in my house.
Despite excellent marks in science classes in school, I still don't fully understand electricity, nor do I really care to. I zapped the shit out of myself trying to change out a faulty light switch back in college, and since then I try to pretend electricity doesn't really exist (not really). Even static electricity shooting out of my fingertips every winter has me firmly believing that the world is constantly trying to electrocute me. My relationship with electricity now solely involves me plugging things carefully into outlets and then turning those things on and off. And as much as I enjoy fixing things, if those things involve wiring or rewiring or anything involving a fuse box, I leave it to the professionals. Because fuck electricity.
Fortunately professional electricians exist. I don't know if these people understand electricity completely, trust it implicitly, or just don't give a shit about the occasional zap that could potentially stop their heart from beating (which, though I am not a cardiologist I understand to be a Very Bad Thing). Irrespective of how or why they do it, they seem more than happy to fiddle with whatever potentially lethal electrical thing has gone awry. Unfortunately, however, not all professional electricians know what the hell they are doing.
"Electrocution" is a portmanteau of "electricity" and "execution" originally coined in the late 19th century to describe death by the electric chair. It has since come to mean any death from electrical shock (as opposed to cardiogenic shock, hypovolemic shock, and "OMG can you believe she's wearing that to a funeral??" shock). Electrical injuries are particularly difficult to treat because they often combine cutaneous thermal injuries (ie burns), internal thermal injuries (including muscle necrosis), cardiac electrical dysrhythmias, and mechanical trauma from the inevitable fall after the shock. Thankfully they are also relatively rare, and most are treated at dedicated burn facilities, which mine is not. Despite this, I still see the occasional electrical injury victim.
Like Lou (not his real name™), who was my patient, and his partner, who was not. Don't worry, I'll explain.
Lou was driving to a job when he heard over his business radio that his partner had suffered a moderate shock while repairing an air conditioning unit in an attic space. Wanting to make sure his buddy was ok, Lou diverted to that establishment, where he found his partner somewhat dazed but relatively unscathed. Apparently his partner hadn't turned off the main power before starting, and at some point he had come into contact with a live wire that was hanging from the ceiling.
Now common sense would dictate either A) your partner turning off the power prior to starting, or B) turning off the power after your partner gets a nasty shock. As you can easily tell, either way the power gets turned off. Right? RIGHT?
Common sense, I am sad to report, is no longer common.
Lou apparently decided to finish the job his partner had started without addressing the live wire hanging from the ceiling that had nearly finished off his partner. He climbed the ladder to the attic space, reached down to get a tool, and as he stood up he caught the live wire with his forehead.
Hilarity did not ensue.
The shock Lou received was significantly greater than his partner's. He was predictably thrown backwards down the ladder where various parts of his anatomy bounced off several steps, ultimately striking his head on the floor below and losing consciousness.
And that is where we pick up his story.
Lou had just started regaining consciousness when he arrived in my trauma bay. He was clearly dazed and confused, a dark electrical burn on his forehead, dried blood matting a good portion of his hair. Surprisingly his main complaint was his right shoulder. A thorough workup demonstrated a fractured clavicle, a scalp laceration, a relatively severe concussion, and a small burn on his forehead (obviously). He had no evidence of a cardiac or skeletal muscle electrical injury, but I watched him overnight just to be sure. He felt much better, though thoroughly ashamed, the next morning when I sent him home.
I get a bit miffed when doctors in other specialties suggest how I do my job, but I admittedly get a rather severe eye twitch when non-doctors do it. Despite this, before Lou left the hospital I felt entirely comfortable reminding him to turn off the goddamned electricity before working on it.
I also made sure to note which company he works for and made a mental note never to hire them. Any professionals working on my power lines need to know what the hell they are doing and, you know, not die in my house.
Monday, 6 November 2017
Texas
I was supposed to be publishing another stupid patient story today. I didn't think I would be writing about this. Again. I thought the death of 58 innocent people in Las Vegas a month ago would be enough to stimulate the United States government to talk about gun control. To at least get a conversation started. I thought surely something, anything would happen, something would get done, some conversation would get initiated in Washington DC that would lead to some kind of change.
Then over the next few weeks, the furor over the shooting withered. Then it died completely. Instead of reading about potential gun control legislation, I read about a new US tax bill that was introduced. Whoopdefucking doo.
And now there is yet another mass shooting in the US, this time in Texas. As of this writing, at least 26 more innocent people are dead after a young man walked into a church and started shooting parishioners. Among the victims are a 5-year-old, the 14-year-old daughter of the church's pastor, and a pregnant mother and three of her children. As shocking as that may be, this isn't even the first mass church shooting in recent memory.
I'm going to repeat that in case you didn't get it the first time: THIS IS NOT EVEN THE FIRST MASS CHURCH SHOOTING IN THE PAST TWO YEARS.
How the hell is this possible? How does the American government allow this to continue, time after time after time?
Because the American public, and their government, just don't get it. Within hours, gun nuts immediately piped up, defending their precious guns.
Really? Is that the best you can do? First of all, you need a licence, registration, and training to operate a car. You need none of those things to buy a gun. Of course you can steal a truck and use it for whatever nefarious purpose you choose, but that doesn't change the fact that you don't need a licence, registration, or training to buy a gun in the United States. That is absolutely unconscionable.
Second of all, cars are essential for everyday life. Guns are not.
Third of all, this guy didn't use a truck. He used this:
Can anyone explain to me why an American citizen needs one of these. Anyone? Are you protecting your family from home invaders with one of these? Are you hunting with one of these? Are you going skeet shooting with one of these? Oh, perhaps this is the reason:
Really? REALLY? Yes, that's how the second amendment reads, because that's what the second amendment was originally about. But this is 2017, not 1791 when that amendment was written. In 2017 the United States government has hundreds of thousands of soldiers in their army, navy, air force, and marines with the most high-tech weaponry on the planet. Oh, and in case you didn't notice, they also have fucking drones. You really think that rifle is going to protect you from drones? Apparently he does:
Then there was this bit of singular stupidity:
So after two horrific mass shootings barely a month apart, surely US politicians are ready to talk about gun control, right? Right?
And President Trump (I still can't believe that phrase is real) said this:
Or twenty six.
Or fifty eight.
Then over the next few weeks, the furor over the shooting withered. Then it died completely. Instead of reading about potential gun control legislation, I read about a new US tax bill that was introduced. Whoopdefucking doo.
And now there is yet another mass shooting in the US, this time in Texas. As of this writing, at least 26 more innocent people are dead after a young man walked into a church and started shooting parishioners. Among the victims are a 5-year-old, the 14-year-old daughter of the church's pastor, and a pregnant mother and three of her children. As shocking as that may be, this isn't even the first mass church shooting in recent memory.
I'm going to repeat that in case you didn't get it the first time: THIS IS NOT EVEN THE FIRST MASS CHURCH SHOOTING IN THE PAST TWO YEARS.
How the hell is this possible? How does the American government allow this to continue, time after time after time?
Because the American public, and their government, just don't get it. Within hours, gun nuts immediately piped up, defending their precious guns.
This seems to be one of their favourites, especially after several people were run over in Edmonton a month ago, in Barcelona back in August, and in New York City a few days ago. On the surface it seems like a valid argument. But if you think about it a little deeper, the argument boils down to "Crazy people who want to kill will find a way to kill. Either ban everything that can kill, or don't ban anything."Sure are we going to ban trucks because some asshat mows folks down with them?? https://t.co/HTN5xxA8p6— FastEddieFelson (@rdeh20) November 5, 2017
Really? Is that the best you can do? First of all, you need a licence, registration, and training to operate a car. You need none of those things to buy a gun. Of course you can steal a truck and use it for whatever nefarious purpose you choose, but that doesn't change the fact that you don't need a licence, registration, or training to buy a gun in the United States. That is absolutely unconscionable.
Second of all, cars are essential for everyday life. Guns are not.
Third of all, this guy didn't use a truck. He used this:
Can anyone explain to me why an American citizen needs one of these. Anyone? Are you protecting your family from home invaders with one of these? Are you hunting with one of these? Are you going skeet shooting with one of these? Oh, perhaps this is the reason:
It's not a bad thing, but what caused it is a bad thing. I believe in the right to own arms to protect yourself from governmental tyranny— Jay Clifton (@jaymclifton) November 5, 2017
Really? REALLY? Yes, that's how the second amendment reads, because that's what the second amendment was originally about. But this is 2017, not 1791 when that amendment was written. In 2017 the United States government has hundreds of thousands of soldiers in their army, navy, air force, and marines with the most high-tech weaponry on the planet. Oh, and in case you didn't notice, they also have fucking drones. You really think that rifle is going to protect you from drones? Apparently he does:
Because according to gun fanatics, the solution isn't just more guns, it's more BIGGER guns. I can't even muster an appropriate response to that. I just can't.If the second amendment wasn't restricted and citizens could own any type of firearm they wished we could overthrow a tyrannical government— Jay Clifton (@jaymclifton) November 5, 2017
Then there was this bit of singular stupidity:
I fed this through my Idiot to English Translation Engine, and this is what came out:You're stupid isn't there a law against murder didn't stop a thing make all the laws you want won't change a thing— Ron Bishop (@RonBish88147167) November 5, 2017
People break laws, so you may as well not even make laws.Which is quite possibly one of the stupidest arguments against gun control I have ever seen and much stupider than my imagination could have ever dreamed up. Anarchy as the solution to crime. Speechless.
So after two horrific mass shootings barely a month apart, surely US politicians are ready to talk about gun control, right? Right?
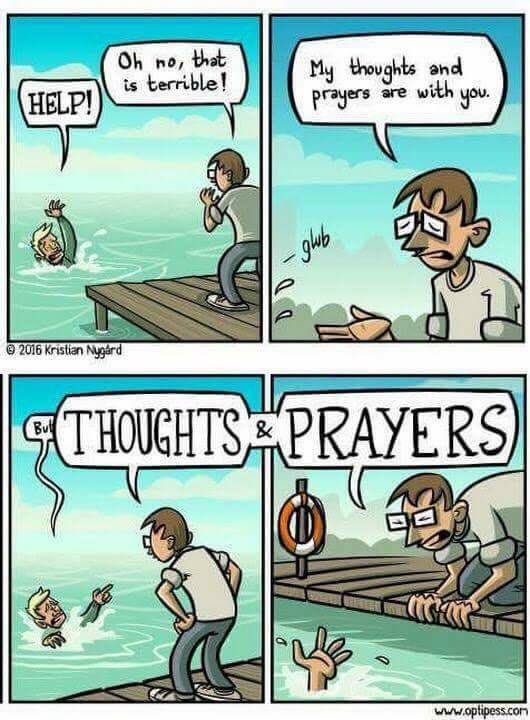
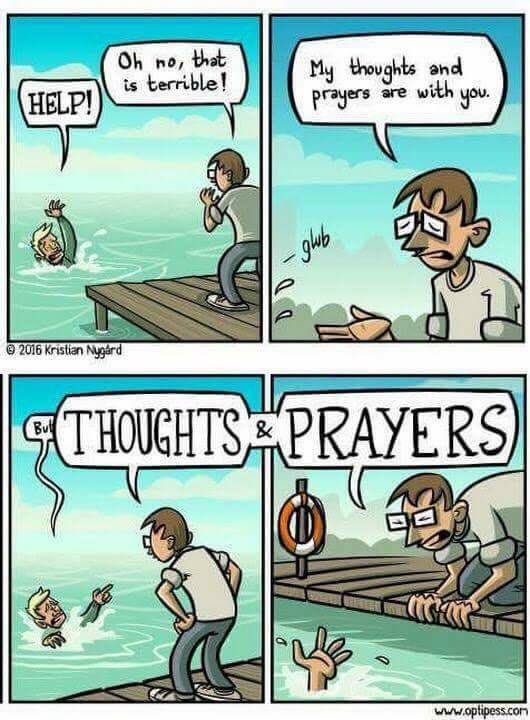
Prayers? These people were at church. They already had prayers. Prayers aren't going to stop mass shootings.Reports out of Texas are devastating. The people of Sutherland Springs need our prayers right now.— Paul Ryan (@SpeakerRyan) November 5, 2017
And President Trump (I still can't believe that phrase is real) said this:
Mental health is your problem here. This isn't a guns situation, this is a mental health problem at the highest level. It's a very, very sad event.Mental health is the issue with any murder, because only an immoral waste of carbon and oxygen would murder another human being. But if you give that waste of carbon and oxygen a gun, you make it much easier to take a life.
Or twenty six.
Or fifty eight.
Monday, 30 October 2017
The Speech
One of my favourite things to do is to lecture people. By "lecture" I don't mean lecturing medical students, which I am unfortunately contractually obligated to do. It turns out I'm a terrible teacher; I just have absolutely no patience for people who just don't get it. Ironically, my backup plan if my medical career fizzled was to be a biology teacher. Yeah . . . that would not have gone well.
No, what I mean is lecturing patients, most notably drunk drivers. I love it. I relish it. I enjoy every opportunity to tell people that what they just did was stupid, reckless (though not wreckless, har har), irresponsible, and their thoughtless act endangered not only their own lives but the lives of everyone around them. In case you can't tell, I have a canned speech in my head that I've used several hundred times, and it keeps getting better every time I give it.
Unfortunately I don't always get to give The Speech. Sometimes the bad guys leave before I get the chance, and rarely there just isn't time. Even more rarely, however, I don't need to.
Like with Edwin (not his real name™).
Being awakened in the middle of the night is a pain in the ass. Not only do I have to shake out the mental cobwebs to make sure I am alert enough to deal with whatever is coming in, I also have to rinse my mouth a bit and make sure my hair doesn't look completely insane. Don't misunderstand, I don't care if I look a bit like Albert Einstein, but trust me when I say you absolutely do not want your trauma surgeon looking like Yahoo Serious. Anyway, when my pager goes off at 3 AM on a Friday night telling me I have a car accident victim on the way, I can be well assured it's a drunk driver.
Enter Edwin the Drunk Driver.
I like to think that Edwin, who was 22-years-stupid, would have been a Type I Drunk had he not been quite as intoxicated as he was. However, with the amount of alcohol in his system, he could barely keep his eyes open let alone yell at people coherently. Everything that did come out of his mouth was mumbled worse than Muttley. I was absolutely astounded he had even been able to find his car keys let alone drive. Though he couldn't really speak, what he could do was fight: with the medics, with us, with literally anyone who came within arm's reach. He had blood on his face which clearly came from somewhere, but he was completely unable to cooperate with any sort of workup. We were therefore forced to sedate him and intubate him to complete (or start) our evaluation.
Once he was sedated the entire team let out a collective huge sigh of relief as the trauma bay immediately quieted. What was most obvious was the relatively small laceration on his forehead which had already stopped bleeding. What hadn't stopped bleeding, however, was his spleen.
His splenic laceration was first diagnosed by a bedside ultrasound and was then confirmed by CT scan. It wasn't the worst I'd ever seen, but it was certainly there. He also had a few minor fractures in his pelvis, none of which would be anything more than really annoying for the next few weeks. But as I was going through his blood work, one number stood out that caused my ire to rise. It was a foregone conclusion that his blood alcohol would be elevated (it was about 4 times the legal limit), but even though the number didn't really surprise me, for some unknown reason it still made me angry.
Actually, no it isn't an unknown reason. The reason is very known. It's because my wife drives my children around on the very roadway Edwin was screaming his way through that night. Edwin put everyone's lives around him at risk, and he was incredibly lucky that only he was injured, luckier still his injuries did not end up being life-threatening.
The Speech was already being prepared in my mind. I just needed to let him sober up overnight. No sense in wasting it on a slurring puddle of whiskey or beer or whatever the hell he had been drinking.
By the following morning, Edwin was sober, awake, and breathing on his own, and the breathing tube had been removed. I stood outside his room readying The Speech with steely resolve, hoping his mother/wife/girlfriend/anyone would be there to hear my scathing lecture. I took one final breath, turned around, and walked in.
What greeted me was not at all what I expected: Edwin, the loud, brash, obnoxious, out-of-control drunk from the night before was talking softly, almost meekly, with his mother, who looked mildly anxious though not angry.
Well . . . that was unexpected.
After perfunctorily asking him how he was feeling ("Sore, doctor"), if he was having any new pain ("No, sir"), and if he remembered anything from the previous night ("No, sir"), I was about to launch into The Speech when he cut across me gently.
"Doctor, did I hurt anyone last night? Is everyone ok?" Tears started to well in his eyes.
My steely resolve was starting to turn into oatmeal.
It only took a minute or two of talking with Edwin to discover that he was truly and genuinely mortified at what he had done and what could have been. The last thing he remembered from the previous night was drinking at the pub, and the next thing he remembered was waking up in his hospital bed this morning. He was terrified he had hurt someone, and he had nothing but regret and remorse behind his eyes.
Yeah yeah, I can already hear a lot of you cynics screaming "But Doc, come on! He was faking it! How could you fall for it? He just feels bad because he wrecked his car!" No. I saw his eyes. This was no act. I see a lot of drunk drivers and I've heard the lot of them tell me how they've never done it before, they'll never do it again, blah blah blah blah. I can see right through the charade, and it doesn't impress me in the least. But Edwin was different. Edwin impressed me. He looked instantly relieved when I told him it no one else was hurt, but he was still visibly shaken.
"That just isn't me, Doc. I don't know why I did that. I just have no idea." The tears continued, real tears of penitence. "I swear that just isn't me. I just have to learn from this, learn from this mistake. Never again. NEVER. This is a real turning point for me, Doc. It has to be. I just don't know what I would have done if I had hurt someone."
And I absolutely believed him.
Edwin was stealing my opportunity to give The Speech, and I let him. He went on for several minutes beating himself up much more effectively than I possibly could have. His mother sat behind him, nodding here and there, wiping a tear away every so often. When he was done he looked up at me.
"At least I didn't hurt anyone. Right?"
I saw Edwin in my office about a week later. He was limping slightly and the swelling around his right eye had almost disappeared, though his black eye had not yet. His laceration had healed well and I removed his sutures. Before I could even bring it up, Edwin said, "Doctor, thank you for taking care of me. I've given up alcohol completely. This was a real wake-up call for me. I just, well, I just wanted to say thank you. Thank you." True remorse is a rare thing for me. But learning from a mistake that quickly is even rarer.
Now before any of you just on my case for being a big softy, don't worry - I got to give The Speech just 2 days later. And I let it rip with no hesitation.
No, what I mean is lecturing patients, most notably drunk drivers. I love it. I relish it. I enjoy every opportunity to tell people that what they just did was stupid, reckless (though not wreckless, har har), irresponsible, and their thoughtless act endangered not only their own lives but the lives of everyone around them. In case you can't tell, I have a canned speech in my head that I've used several hundred times, and it keeps getting better every time I give it.
Unfortunately I don't always get to give The Speech. Sometimes the bad guys leave before I get the chance, and rarely there just isn't time. Even more rarely, however, I don't need to.
Like with Edwin (not his real name™).
Being awakened in the middle of the night is a pain in the ass. Not only do I have to shake out the mental cobwebs to make sure I am alert enough to deal with whatever is coming in, I also have to rinse my mouth a bit and make sure my hair doesn't look completely insane. Don't misunderstand, I don't care if I look a bit like Albert Einstein, but trust me when I say you absolutely do not want your trauma surgeon looking like Yahoo Serious. Anyway, when my pager goes off at 3 AM on a Friday night telling me I have a car accident victim on the way, I can be well assured it's a drunk driver.
Enter Edwin the Drunk Driver.
I like to think that Edwin, who was 22-years-stupid, would have been a Type I Drunk had he not been quite as intoxicated as he was. However, with the amount of alcohol in his system, he could barely keep his eyes open let alone yell at people coherently. Everything that did come out of his mouth was mumbled worse than Muttley. I was absolutely astounded he had even been able to find his car keys let alone drive. Though he couldn't really speak, what he could do was fight: with the medics, with us, with literally anyone who came within arm's reach. He had blood on his face which clearly came from somewhere, but he was completely unable to cooperate with any sort of workup. We were therefore forced to sedate him and intubate him to complete (or start) our evaluation.
Once he was sedated the entire team let out a collective huge sigh of relief as the trauma bay immediately quieted. What was most obvious was the relatively small laceration on his forehead which had already stopped bleeding. What hadn't stopped bleeding, however, was his spleen.
His splenic laceration was first diagnosed by a bedside ultrasound and was then confirmed by CT scan. It wasn't the worst I'd ever seen, but it was certainly there. He also had a few minor fractures in his pelvis, none of which would be anything more than really annoying for the next few weeks. But as I was going through his blood work, one number stood out that caused my ire to rise. It was a foregone conclusion that his blood alcohol would be elevated (it was about 4 times the legal limit), but even though the number didn't really surprise me, for some unknown reason it still made me angry.
Actually, no it isn't an unknown reason. The reason is very known. It's because my wife drives my children around on the very roadway Edwin was screaming his way through that night. Edwin put everyone's lives around him at risk, and he was incredibly lucky that only he was injured, luckier still his injuries did not end up being life-threatening.
The Speech was already being prepared in my mind. I just needed to let him sober up overnight. No sense in wasting it on a slurring puddle of whiskey or beer or whatever the hell he had been drinking.
By the following morning, Edwin was sober, awake, and breathing on his own, and the breathing tube had been removed. I stood outside his room readying The Speech with steely resolve, hoping his mother/wife/girlfriend/anyone would be there to hear my scathing lecture. I took one final breath, turned around, and walked in.
What greeted me was not at all what I expected: Edwin, the loud, brash, obnoxious, out-of-control drunk from the night before was talking softly, almost meekly, with his mother, who looked mildly anxious though not angry.
Well . . . that was unexpected.
After perfunctorily asking him how he was feeling ("Sore, doctor"), if he was having any new pain ("No, sir"), and if he remembered anything from the previous night ("No, sir"), I was about to launch into The Speech when he cut across me gently.
"Doctor, did I hurt anyone last night? Is everyone ok?" Tears started to well in his eyes.
My steely resolve was starting to turn into oatmeal.
It only took a minute or two of talking with Edwin to discover that he was truly and genuinely mortified at what he had done and what could have been. The last thing he remembered from the previous night was drinking at the pub, and the next thing he remembered was waking up in his hospital bed this morning. He was terrified he had hurt someone, and he had nothing but regret and remorse behind his eyes.
Yeah yeah, I can already hear a lot of you cynics screaming "But Doc, come on! He was faking it! How could you fall for it? He just feels bad because he wrecked his car!" No. I saw his eyes. This was no act. I see a lot of drunk drivers and I've heard the lot of them tell me how they've never done it before, they'll never do it again, blah blah blah blah. I can see right through the charade, and it doesn't impress me in the least. But Edwin was different. Edwin impressed me. He looked instantly relieved when I told him it no one else was hurt, but he was still visibly shaken.
"That just isn't me, Doc. I don't know why I did that. I just have no idea." The tears continued, real tears of penitence. "I swear that just isn't me. I just have to learn from this, learn from this mistake. Never again. NEVER. This is a real turning point for me, Doc. It has to be. I just don't know what I would have done if I had hurt someone."
And I absolutely believed him.
Edwin was stealing my opportunity to give The Speech, and I let him. He went on for several minutes beating himself up much more effectively than I possibly could have. His mother sat behind him, nodding here and there, wiping a tear away every so often. When he was done he looked up at me.
"At least I didn't hurt anyone. Right?"
I saw Edwin in my office about a week later. He was limping slightly and the swelling around his right eye had almost disappeared, though his black eye had not yet. His laceration had healed well and I removed his sutures. Before I could even bring it up, Edwin said, "Doctor, thank you for taking care of me. I've given up alcohol completely. This was a real wake-up call for me. I just, well, I just wanted to say thank you. Thank you." True remorse is a rare thing for me. But learning from a mistake that quickly is even rarer.
Now before any of you just on my case for being a big softy, don't worry - I got to give The Speech just 2 days later. And I let it rip with no hesitation.
Thursday, 19 October 2017
Who am I
Instead of a stupid patient story this week, I've decided to play a game with you, my loyal (and disloyal and peripatetic) readers. No damn it, I don't mean we're going to play a game like Jigsaw, nor are we going to play Global Thermonuclear War. No, a normal game. A kid's game, actually. Remember "Who am I"? Perhaps it had a different name when (and where) you played it, but the rules are always the same: I will tell you a series of facts about something or someone, and you have to guess who I am.
I have a feeling this little experiment will go swimmingly. If you think you know the answer, please refrain from shouting out your guess so that others can continue to play.
Ready?
Let's play.
I have a feeling this little experiment will go swimmingly. If you think you know the answer, please refrain from shouting out your guess so that others can continue to play.
Ready?
Let's play.
- I am not a person, but rather a thing.
- I was invented not too long ago to help prevent a major cause of death and injury.
- Millions of people use me regularly, and most do not give me a second thought.
- Proper use of me only takes a couple of seconds and is not uncomfortable when applied properly.
- I am very safe when used properly, but I can be misused.
- I am exceedingly effective at protecting people's lives.
- Use of me is strongly recommended everywhere around the world and is even mandated in some places.
- Despite the fact that there are many laws around the world regarding mandatory use of me, some people still eschew me and choose not to use me.
- There are very few real reasons not to use me.
- There are several more recently developed items that have been invented and found to make use of me more effective.
- Despite my excellent safety profile, there are rare instances where I can cause major injury or even death.
- Because I can rarely hurt people, some believe I am evil and will always refuse me.
- People who are against me actually think they are safer without me.
Are we getting any ideas here? Yes? No? Do you need more time to think?
Well if you guessed SEAT BELTS, then you are CORRECT!
What? What do you mean you weren't thinking I was seat belts! Wait wait wait, you weren't thinking I was VACCINES, were you?
Hm . . . well now that I read my description back, it sure does sound like I could be vaccines, doesn't it.
You are correct; that wasn't a question.
This stupid little game was inspired by some stupid little tweets that I've read over the past week or so regarding the flu vaccine, including this humourous little gem:
While the vast majority of the 200+ responses to my tweet were supportive, some of them were less than enthusiastic. Ok, that's putting it mildly. I'll change that to "complete bullshit".
No, seriously. "My own immune system". I can't even make this shit up.
Others groused about the nurse's informed consent:
Then there were multiple people claiming this:
NO. No it absolutely can not. If you take nothing else away from this stupid blog post, take away this: it is a 100% biological impossibility to catch the flu from the flu shot. End of. Full stop. PERIOD. Before you rush down to the comments to say "BUT THE FLU MIST IS A LIVE VIRUS VACCINE YOUR STUPID LOL", I didn't say the flu vaccine, I said the flu shot, which is an inactivated (read: dead) virus vaccine. The flu mist is a live attenuated vaccine which has unfortunately not been nearly as successful as anyone had hoped. Regardless, You can't catch the flu from a flu shot, you can't transmit it to others, and it doesn't fucking shed. You may feel crummy for a day or two due to the immune response, but that is NOT the flu, which knocks you on your ass for a week or two and may fucking kill you.
Now I will be the first to admit that the flu shot mostly sucks. I don't mean getting it sucks, because just like Donald Trump, it's a tiny little prick. As I mentioned in my stupid little game, it has an excellent safety profile. No, what I mean is that compared to all other vaccines, it just doesn't work as well. Compared to MMR (97% effective with 2 doses), polio (99% effective with 3 doses), Haemophilus influenza (95% effective with 3 doses), and meningitis (85-100% effective with 3 doses), the flu vaccine just doesn't quite stack up:
It sure is easy to denigrate such terrible-looking results. I mean, just look at 2014-2015 when the flu shot was just 20% effective! And for fuck's sake, in 2004-2005 it was less than 10% effective! Why the hell do we even fucking bother with this shit?
The reason we fucking bother with this shit is because it DOES work sometimes, and that is better than nothing. Even if it is only 10% effective, that is 10% higher than ZERO PERCENT. The flu kills thousands of people every year and happens to target the most vulnerable of our population (children, elderly, sick), so it is NOT just a bad cold. The flu shot is extremely safe, with fleetingly rare reports of serious adverse events at a rate of around 1 per 1.4 million doses. Plus, in some years the effectiveness approaches 60%, which is actually pretty goddamned good. And the flu vaccine has also been found to decrease both the severity and mortality of pneumonia during flu season.
The bottom line is this: influenza is not just a bad cold. The flu sucks. The flu shot works (sometimes). The flu shot is safe. The flu shot is inexpensive. And the flu shot does not give you the flu.
So if you are a child, a healthcare worker, an elderly person, are pregnant, or have a chronic medical condition,
What? What do you mean you weren't thinking I was seat belts! Wait wait wait, you weren't thinking I was VACCINES, were you?
Hm . . . well now that I read my description back, it sure does sound like I could be vaccines, doesn't it.
You are correct; that wasn't a question.
This stupid little game was inspired by some stupid little tweets that I've read over the past week or so regarding the flu vaccine, including this humourous little gem:
But that's from noted lunatic and all-around asshole Mike Adams, so I mostly let that go. Not really:All #vaccine research eventually leads to Bill Gates and Nazi #eugenics https://t.co/eISiQARpo7 #antivax— HealthRanger (@HealthRanger) October 12, 2017
Waste of skin. Heh. But the one that really got to me was this one:You are an odious waste of skin, and I rue the fact that I am forced to share oxygen with you.— Doc Bastard (@DocBastard) October 12, 2017
Delete your account. @HealthRanger https://t.co/5myG3qq8lV
I wish I could remember where on Facebook I found that, but in case you can't see the picture it is a nurse bleating about the fact that she is being forced to wear a mask because she refused a flu shot. What this nurse apparently forgot is that nurses are on the front line when it comes to patient protection, and they should be first in line to get their goddamned flu shot. Because this isn't about you and your stupid hurt feelings madam, it's about not transmitting a potentially fatal disease to the most vulnerable people for whom you have chosen to care.This nurse claims she's being "shamed" for refusing a flu shot.— Doc Bastard (@DocBastard) October 14, 2017
If you don't understand protecting patients, get the fuck out of medicine. pic.twitter.com/uJP7Eaa6br
While the vast majority of the 200+ responses to my tweet were supportive, some of them were less than enthusiastic. Ok, that's putting it mildly. I'll change that to "complete bullshit".
No, seriously. "My own immune system". I can't even make this shit up.
Others groused about the nurse's informed consent:
Let me assure you that we all sign informed consent forms prior to receiving the vaccine, and they say the same things it says on the consent forms that the general public signs. And making a nurse wear a mask doesn't violate her privacy, and it doesn't violate informed consent. I have a sneaking suspicion that when she was hired (or when her hospital adopted a mandatory flu shot policy) she signed a form acknowledging that she would either get the shot or wear a mask.Informed consent has been thrown out the window for a shitty 60y.o. vaccine based on shitty science. But if badgering makes you feel good..— Demo Schopenheimer (@schopenheimer) October 14, 2017
Then there were multiple people claiming this:
Not true. The flu vaccine can cause the flu or flu-like symptoms.— Scary Kelly 🦇 (@arcadek3lly) October 15, 2017
NO. No it absolutely can not. If you take nothing else away from this stupid blog post, take away this: it is a 100% biological impossibility to catch the flu from the flu shot. End of. Full stop. PERIOD. Before you rush down to the comments to say "BUT THE FLU MIST IS A LIVE VIRUS VACCINE YOUR STUPID LOL", I didn't say the flu vaccine, I said the flu shot, which is an inactivated (read: dead) virus vaccine. The flu mist is a live attenuated vaccine which has unfortunately not been nearly as successful as anyone had hoped. Regardless, You can't catch the flu from a flu shot, you can't transmit it to others, and it doesn't fucking shed. You may feel crummy for a day or two due to the immune response, but that is NOT the flu, which knocks you on your ass for a week or two and may fucking kill you.
Now I will be the first to admit that the flu shot mostly sucks. I don't mean getting it sucks, because just like Donald Trump, it's a tiny little prick. As I mentioned in my stupid little game, it has an excellent safety profile. No, what I mean is that compared to all other vaccines, it just doesn't work as well. Compared to MMR (97% effective with 2 doses), polio (99% effective with 3 doses), Haemophilus influenza (95% effective with 3 doses), and meningitis (85-100% effective with 3 doses), the flu vaccine just doesn't quite stack up:
It sure is easy to denigrate such terrible-looking results. I mean, just look at 2014-2015 when the flu shot was just 20% effective! And for fuck's sake, in 2004-2005 it was less than 10% effective! Why the hell do we even fucking bother with this shit?
The reason we fucking bother with this shit is because it DOES work sometimes, and that is better than nothing. Even if it is only 10% effective, that is 10% higher than ZERO PERCENT. The flu kills thousands of people every year and happens to target the most vulnerable of our population (children, elderly, sick), so it is NOT just a bad cold. The flu shot is extremely safe, with fleetingly rare reports of serious adverse events at a rate of around 1 per 1.4 million doses. Plus, in some years the effectiveness approaches 60%, which is actually pretty goddamned good. And the flu vaccine has also been found to decrease both the severity and mortality of pneumonia during flu season.
The bottom line is this: influenza is not just a bad cold. The flu sucks. The flu shot works (sometimes). The flu shot is safe. The flu shot is inexpensive. And the flu shot does not give you the flu.
So if you are a child, a healthcare worker, an elderly person, are pregnant, or have a chronic medical condition,
Monday, 9 October 2017
Fool me once again
I've written before about not learning from mistakes. In case you missed that episode, please go back and read it. I just did, and that story is fucking hilarious (if I do say so myself).
Anyway, it seems that in my trauma bay I see more than my fair share of people who are either unwilling or unable to learn from what they've done wrong so that they don't do it again. Everyone makes misteaks (myself included, naturally), but unlike many of my patients I try to refrain from making the same misteak twice. This is a lesson that I beat into my children (NOT LITERALLY) on a daily basis. After all, I tell them, if you don't learn from your mistakes, then what the hell is the point of making mistakes. Right? Of course right.
I have to assume that Lacey (not her real name™) didn't have such caring and knowledgeable parents.
Lacey was brought to me in a bit of a heap one fine late evening, the police trailing just behind. That is, as you have probably guessed, never a good sign. When she was wheeled into the trauma bay, she was completely unresponsive, unable even to open her eyes. When I see such a patient, I think of the three Most Likely Possibilities:
Wait, you . . . what? Of course you did. Somehow, that made total and complete sense.
Unfortunately for the general public, the police left without arresting her. I have no idea why and no reasonable suspicion other than that the officer got bored of waiting for Lacey to wake up. So instead of going to jail for endangering every single person around her, Lacey got away with it. Again. She woke up, got dressed, asked me for a prescription for narcotics (HA!), and went home.
I can guarantee that she learned absolutely nothing from this episode, and I can further guarantee with near 100% precision that I will see her again. Probably soon.
Anyway, it seems that in my trauma bay I see more than my fair share of people who are either unwilling or unable to learn from what they've done wrong so that they don't do it again. Everyone makes misteaks (myself included, naturally), but unlike many of my patients I try to refrain from making the same misteak twice. This is a lesson that I beat into my children (NOT LITERALLY) on a daily basis. After all, I tell them, if you don't learn from your mistakes, then what the hell is the point of making mistakes. Right? Of course right.
I have to assume that Lacey (not her real name™) didn't have such caring and knowledgeable parents.
Lacey was brought to me in a bit of a heap one fine late evening, the police trailing just behind. That is, as you have probably guessed, never a good sign. When she was wheeled into the trauma bay, she was completely unresponsive, unable even to open her eyes. When I see such a patient, I think of the three Most Likely Possibilities:
- She has a severe brain injury,
- She is drunk (or otherwise intoxicated) as hell,
- She is faking to avoid talking to the police.
It's my job to differentiate among the three.
"Evening, Doc. Here we have Lacey. She's 29, history of anxiety and depression, allergy to penicillin, takes one medication for anxiety though she doesn't know which one. History of heroin abuse. We found her like this, unresponsive, outside her car on the side of the road. Basically no damage to the car, but, you know, we can't tell if she hit her head or oh-deed or what. She's been unresponsive like this since we found her, though her vitals have been rock stable."
A quick glance at Lacey revealed no outward sign of trauma, not even an abrasion. She literally had not a single scratch on her. I strongly suspected Most Likely Possibility #2. She had a grossly abnormal neurological exam: her pupils were pinpoint and she did not respond to painful stimuli, so I could rule out Most Likely Possibility #3 (though #1 was very much still in play). Her physical exam was otherwise completely normal. X-rays of her chest and pelvis were normal. An ultrasound of her chest and abdomen showed no sign of bleeding around her heart, lungs, liver, spleen, kidneys, or bladder. A full-body CT scan was negative.
This did not seem to be Most Likely Possibility #1 either. Shocking.
A few minutes after seeing her normal scans, her lab work finally came back. Her chemistry and complete blood count were (are you sitting down?) totally normal. Finally I saw what I was looking for: something. Something. Anything that could explain why she was out cold.
Her urine tox screen was positive for heroin. I hate the term "Duh", but really. DUH.
Now clearly no one in the trauma bay was surprised, but as we started to discuss the sheer stupidity of driving after injecting way-too-much heroin (though to be fair, any amount of heroin is way too much if you plan on driving), something occurred to me about the medics' presentation that hopefully occurred to you too. I cocked my head as I thought about it, wondering.
Fortunately the ambulance crew was still milling around the hallway, so I decided to ask them the question that was noodling around my brain: If she was unresponsive when you found her, how the hell did you know her medical history other than heroin use and that she was allergic to penicillin??
The medics turned to each other, laughed, turned back to me, laughed in my face, and then started high-fiving each other. Not really, but that's what it felt like as he chuckled politely and said,
"Oh, because we picked Lacey up for a heroin overdose earlier this morning too."
Wait, you . . . what? Of course you did. Somehow, that made total and complete sense.
Unfortunately for the general public, the police left without arresting her. I have no idea why and no reasonable suspicion other than that the officer got bored of waiting for Lacey to wake up. So instead of going to jail for endangering every single person around her, Lacey got away with it. Again. She woke up, got dressed, asked me for a prescription for narcotics (HA!), and went home.
I can guarantee that she learned absolutely nothing from this episode, and I can further guarantee with near 100% precision that I will see her again. Probably soon.
Tuesday, 3 October 2017
Guns
I'm angry.
I'm sad.
I'm thoroughly upset.
If you don't know what I'm talking about, go google "Las Vegas" right now and you'll be instantly updated. If you're reading this after October 2017, well, just click here I guess.
A man whom I will not name went on a shooting rampage from an elevated vantage point in Las Vegas, killing 59 people (so far, not including himself) and injuring about 500. I will repeat: HE KILLED 59 INNOCENT PEOPLE AND INJURED OVER 500 MORE. In an hour. With an arsenal of guns.
All of which were obtained legally.
In addition to the 23 guns found in his hotel room, police found 19 more firearms in his home along with several thousand rounds of ammunition. A terrorist, right? A maniac with a long history of mental illness, right? A career criminal who got all the guns illegally, right?
NO. He was a wealthy gambler who purchased these guns legally. All of them. He had no criminal background. He passed an FBI background check. And he was able to amass an arsenal and then kill several dozen people with it.
And predictably, infuriatingly, people are defending his right to do so.
As someone who deals with gun violence on a daily basis, I am sick to fucking death of people (looking at you, 'Muricans) shouting about their second amendment rights. Their right to defend themselves. Their right to own a gun.
Yes, you have the right to bear arms, just like others have the first amendment right to say "FUCK YOU" for it. But for those of you about to comment to that effect, that amendment you seem to idolise was written in 1791 when guns were fucking muskets and took 5 minutes to reload. Do you think your founding fathers would have been ok with semi-automatic rifles being converted into automatic rifles with legally purchased parts? Do you think they would have passed that law knowing what we have now, knowing that a rifle can be purchased online in less time than it takes to reload a musket?
And above all, do you really think that law can't be changed?
IT'S CALLED A FUCKING 'AMENDMENT'! OF COURSE IT CAN BE CHANGED!
And as for your right to protect yourself, give me a fucking break. Look at the actual statistics. For every "protection" gun death in the US, there are 34 gun-related homicides and 78 gun-related suicides. You don't even have to look it up, because I've done the work for you. Just click anywhere in this paragraph Those are FBI statistics. Read them. Understand them. Yes, guns protect people, but at a very high cost.
The second amendment was written so that the people could protect themselves against a tyrannical government. When was the last time the second amendment protected the people of the United States against the government? When? Any gun advocates care to answer that one?
FUCKING NEVER. (No, the Whiskey Rebellion doesn't fucking count. Not a single shot was fired, and the people were protesting a tax on alcohol that they didn't like. And even if it did count, that was also way back in 1791. Muskets, remember? And neither does the American Civil War, because the South was trying to fucking defend slavery. And they rightfully fucking lost. And if you'd like to bring up Cliven Bundy, just don't. He was wrong, and he also lost.)
I'm not even going to expound on gun violence in Australia, where over 650,000 guns were bought back by the government after the Port Arthur massacre in 1996, and there have been a total of ZERO mass shootings since then. In contrast, in the US I can think of at least a dozen mass shootings in the past year alone (SO FAR), and a dozen more last year. Is the US the same as Australia? No. Do I think the same policy adopted in Australia would work in the US? YES I DO. And do I have evidence to back up this belief?
YES I FUCKING DO.
Now do I think banning all guns is the answer? Of fucking course not. First off, anyone who thinks that it is even remotely feasible to go out and round up even 1% of the 350 million guns in the US is a certified lunatic. Let's be honest, just changing the law would be difficult enough, and rounding up any guns would be nigh-on impossible. But the state of affairs as it stands now is absolutely untenable, and I categorically refuse to believe that tougher restrictions wouldn't lead to less access to guns, and that less access to guns wouldn't lead to fewer gun deaths.
One final thing. I am sick to fucking death of everyone's "thoughts and prayers" for the victims. I'm tired of hearing about vigils. I've had it with moments of silence. I've never seen a thought or a prayer stop a mass murderer. Vigils don't mean jack shit. I've never heard of silence changing a law. It is WAY PAST TIME for American politicians be silent. It is time for them to stop the thoughts, ignore the prayers, give up the goddamned moments of silence, and GET UP AND DO SOMETHING.
Note: I realise that I will rile approximately 50% of the population with this, and I am absolutely 100% fine with that. I hate guns. Gun owners and fanatics are free to leave whatever comment you like. I understand that you can be rabid in your defence of guns and gun ownership. But understand that I will delete any comment I deem inappropriate.
I'm sad.
I'm thoroughly upset.
If you don't know what I'm talking about, go google "Las Vegas" right now and you'll be instantly updated. If you're reading this after October 2017, well, just click here I guess.
A man whom I will not name went on a shooting rampage from an elevated vantage point in Las Vegas, killing 59 people (so far, not including himself) and injuring about 500. I will repeat: HE KILLED 59 INNOCENT PEOPLE AND INJURED OVER 500 MORE. In an hour. With an arsenal of guns.
All of which were obtained legally.
In addition to the 23 guns found in his hotel room, police found 19 more firearms in his home along with several thousand rounds of ammunition. A terrorist, right? A maniac with a long history of mental illness, right? A career criminal who got all the guns illegally, right?
NO. He was a wealthy gambler who purchased these guns legally. All of them. He had no criminal background. He passed an FBI background check. And he was able to amass an arsenal and then kill several dozen people with it.
And predictably, infuriatingly, people are defending his right to do so.
As someone who deals with gun violence on a daily basis, I am sick to fucking death of people (looking at you, 'Muricans) shouting about their second amendment rights. Their right to defend themselves. Their right to own a gun.
Yes, you have the right to bear arms, just like others have the first amendment right to say "FUCK YOU" for it. But for those of you about to comment to that effect, that amendment you seem to idolise was written in 1791 when guns were fucking muskets and took 5 minutes to reload. Do you think your founding fathers would have been ok with semi-automatic rifles being converted into automatic rifles with legally purchased parts? Do you think they would have passed that law knowing what we have now, knowing that a rifle can be purchased online in less time than it takes to reload a musket?
And above all, do you really think that law can't be changed?
IT'S CALLED A FUCKING 'AMENDMENT'! OF COURSE IT CAN BE CHANGED!
And as for your right to protect yourself, give me a fucking break. Look at the actual statistics. For every "protection" gun death in the US, there are 34 gun-related homicides and 78 gun-related suicides. You don't even have to look it up, because I've done the work for you. Just click anywhere in this paragraph Those are FBI statistics. Read them. Understand them. Yes, guns protect people, but at a very high cost.
The second amendment was written so that the people could protect themselves against a tyrannical government. When was the last time the second amendment protected the people of the United States against the government? When? Any gun advocates care to answer that one?
FUCKING NEVER. (No, the Whiskey Rebellion doesn't fucking count. Not a single shot was fired, and the people were protesting a tax on alcohol that they didn't like. And even if it did count, that was also way back in 1791. Muskets, remember? And neither does the American Civil War, because the South was trying to fucking defend slavery. And they rightfully fucking lost. And if you'd like to bring up Cliven Bundy, just don't. He was wrong, and he also lost.)
I'm not even going to expound on gun violence in Australia, where over 650,000 guns were bought back by the government after the Port Arthur massacre in 1996, and there have been a total of ZERO mass shootings since then. In contrast, in the US I can think of at least a dozen mass shootings in the past year alone (SO FAR), and a dozen more last year. Is the US the same as Australia? No. Do I think the same policy adopted in Australia would work in the US? YES I DO. And do I have evidence to back up this belief?
YES I FUCKING DO.
Now do I think banning all guns is the answer? Of fucking course not. First off, anyone who thinks that it is even remotely feasible to go out and round up even 1% of the 350 million guns in the US is a certified lunatic. Let's be honest, just changing the law would be difficult enough, and rounding up any guns would be nigh-on impossible. But the state of affairs as it stands now is absolutely untenable, and I categorically refuse to believe that tougher restrictions wouldn't lead to less access to guns, and that less access to guns wouldn't lead to fewer gun deaths.
One final thing. I am sick to fucking death of everyone's "thoughts and prayers" for the victims. I'm tired of hearing about vigils. I've had it with moments of silence. I've never seen a thought or a prayer stop a mass murderer. Vigils don't mean jack shit. I've never heard of silence changing a law. It is WAY PAST TIME for American politicians be silent. It is time for them to stop the thoughts, ignore the prayers, give up the goddamned moments of silence, and GET UP AND DO SOMETHING.
Note: I realise that I will rile approximately 50% of the population with this, and I am absolutely 100% fine with that. I hate guns. Gun owners and fanatics are free to leave whatever comment you like. I understand that you can be rabid in your defence of guns and gun ownership. But understand that I will delete any comment I deem inappropriate.
Monday, 18 September 2017
Listen to me
There is a nearly 100% chance that I know more about trauma and trauma surgery than you. I fully realize how arrogant that sounds, but if you think about it for one second hopefully you'll understand why I say it. Having studied for several years in university, several more years of medical school, over half a decade of surgical training, followed by {redacted} years of surgical/trauma practice, hopefully I know a hell of a lot about surgery. Actually now that I think about it, if I don't know more than you about trauma surgery, then my patients have a real problem.
Unless of course you also happen to be a trauma surgeon, in which case hi! Welcome!
Because most people see the white coat as a symbol of an authority figure, I rarely get questioned on my orders and recommendations. Most of the time people nod and say something to the effect of "Yes, doctor." Don't get me wrong, I don't expect people to take everything I say at 100% face value, because as this blog has demonstrated I am most assuredly not always right. Though I don't expect blind adherence, what I do expect is for my patients to listen to me.
Since I don't do kids, all of my patients are adults with adult brains (relatively speaking), so they are (unfortunately) free to listen to what I have to say and then make up their own mind. Tragically, some of those minds are just plain stupid.
The Thursday in question was just like any other typical Thursday, in that everybody seemed to be getting assaulted. I don't know if there was a knife show in town or if the government was spraying everybody with DocBastard's Super Aggression Chemtrails® again, but it seemed that everyone was getting stabbed, punched, or shot, Oliver included.
Oliver (not his real name™) was my second penetrating trauma victim of the day (the first will be found in a future post as well). He had reportedly been stabbed by Some Dude for Some Reason with Some Weapon at Some Point in the past hour. The medics were not terribly forthcoming with details, because Oliver would not tell them anything.
"Hey Doc, this is Oliver. 20 years old. Single stab wound to the left lower chest. Breath sounds have been equal, and he has been calm and cooperative although not talking much. Vital signs are all stable." By the time the medics finished their story, Oliver had already been hooked up to the monitors. His heart rate was 61, his blood pressure was 118/68, and his oxygen saturation was 100% on room air. Hm, I thought, he can't be too seriously injured, because vitals can't get much better than that.
As the medics correctly reported, Oliver had a single 5 cm stab wound to the left lateral chest just where it meets the abdomen. These thoracoabdominal injuries can be a diagnostic and therapeutic nightmare, as the knife could potentially have penetrated anything in his left chest (including lung, heart, and/or great vessels) or anything in the abdomen (including colon, small intestine, stomach, spleen, and diaphragm).
Shit.
So I did what I always do in this situation – I put my finger in the hole. Oliver was clearly unhappy with this manoeuvre, but the laceration was quite deep, extending towards his midsection underneath his 12th rib. I could not feel any obvious penetration into his chest or abdomen, but unfortunately knife blades tend to be thinner than my finger, so this is not a perfect test in any way. Since all of his vital signs remained rock stable, his next stop (after a normal chest x-ray) was the CT scanner. Much to my surprise and chagrin, though the scan did not show any injury in the chest, it did show a small amount of fluid (read: blood) in the left upper abdomen along with a few dots of air where they did not belong.
Shit!
While the air could have come from the outside world, it was more likely to be leaking out from a hollow organ (ie stomach, small intestine, or colon). However, not wanting to base my decision solely on a picture on a computer screen, I went back to examine Oliver, whose vital signs were still completely normal (and probably better than mine at that moment). His abdomen was still soft, flat, and completely nontender (except at the stab wound). At this point my options were:
Ninety minutes later I had a laparoscope in his abdomen, where I was able to see a small amount of blood in the left upper abdomen as well as a small laceration to his diaphragm.
Wait wait wait Doc, 90 minutes? Why the hell did it take you 90 minutes to get him to theatre? That's malpractice! I'm going to report you etc etc.
Hold on there, bucko. Remember how I said Oliver was my second penetrating trauma of the day? Well the first one came in exactly two minutes before Oliver did. He was much sicker than Oliver was, so I had to take him to theatre first. Remember also when I said he would be addressed in a future post? He will. I just haven't gotten to it yet. So hold onto your stupid report and stick it somewhere dark.
Anyway, the diaphragm laceration certainly needed to be repaired, but I also need to make sure nothing else had a hole in it that needed repair. I remove the laparoscope and opened him up the old fashioned way, but after an exhaustive search the only other injury I found was a very small laceration to his omentum. The air on the CT scan had indeed come from the outside world, but assuming that without doing surgery is a potentially lethal mistake. Fortunately for Oliver this was the best possible outcome – his postoperative course should be short, about two to three days, and hopefully uneventful.
Hopefully. (Foreshadowing . . .)
I heaved a big sigh and repaired his diaphragm, everybody gave each other a high-five for a job well done (not really), and I closed. I went to see Oliver the next morning at 7 AM, and he was putting his clothes on, getting ready to leave. You know, 12 hours after major surgery.
Uh . . .
"Oh hey Doc. Listen, I got to go. I have things I need to do at home," he told me with a small wince of pain as he buttoned his shirt. I looked at him sternly and then very slowly and carefully and using very small words explained to him that he just had major surgery 12 hours earlier, and he should expect to be in the hospital for 2 to 3 more days. But Oliver would have nothing of it.
"Nope, sorry I got things I gotta do at home. I've been walking, I feel fine, I need to go." I heaved a very heavy sigh, looked at him even sternlier (yes, that should totally be a word), and explained everything that I had just explained, this time a bit more slowly, a bit more forcefully, and using even smaller words so that he would be sure to understand.
Nope. The nurse called me an hour later to alert me that he had indeed left the hospital against medical advice.
And then one of the emergency physicians called me seven hours after that to tell me that he was back.
Of course.
When I went in to see him the following morning, he looked only mildly abashed, like he had barely done anything wrong. "Welcome back," I told him with a scowl. "Yeah, I probably shouldn't have left, right?" he said, finally looking up from his mobile.
"Right," I told him in that same stern voice I had used before. "That was a stupid thing to do. Really stupid. I expect you to stay here in hospital this time until I discharge you. Clear?" He simply nodded and went back to playing a game on his mobile.
As expected, Oliver had normal post-laparotomy pain which is best treated, you know, in a hospital. He stayed in hospital for 3 more days until his bowels woke back up (which is normal after major abdominal surgery), and he then went home again.
But not until I discharged him.
Unless of course you also happen to be a trauma surgeon, in which case hi! Welcome!
Because most people see the white coat as a symbol of an authority figure, I rarely get questioned on my orders and recommendations. Most of the time people nod and say something to the effect of "Yes, doctor." Don't get me wrong, I don't expect people to take everything I say at 100% face value, because as this blog has demonstrated I am most assuredly not always right. Though I don't expect blind adherence, what I do expect is for my patients to listen to me.
Since I don't do kids, all of my patients are adults with adult brains (relatively speaking), so they are (unfortunately) free to listen to what I have to say and then make up their own mind. Tragically, some of those minds are just plain stupid.
The Thursday in question was just like any other typical Thursday, in that everybody seemed to be getting assaulted. I don't know if there was a knife show in town or if the government was spraying everybody with DocBastard's Super Aggression Chemtrails® again, but it seemed that everyone was getting stabbed, punched, or shot, Oliver included.
Oliver (not his real name™) was my second penetrating trauma victim of the day (the first will be found in a future post as well). He had reportedly been stabbed by Some Dude for Some Reason with Some Weapon at Some Point in the past hour. The medics were not terribly forthcoming with details, because Oliver would not tell them anything.
"Hey Doc, this is Oliver. 20 years old. Single stab wound to the left lower chest. Breath sounds have been equal, and he has been calm and cooperative although not talking much. Vital signs are all stable." By the time the medics finished their story, Oliver had already been hooked up to the monitors. His heart rate was 61, his blood pressure was 118/68, and his oxygen saturation was 100% on room air. Hm, I thought, he can't be too seriously injured, because vitals can't get much better than that.
As the medics correctly reported, Oliver had a single 5 cm stab wound to the left lateral chest just where it meets the abdomen. These thoracoabdominal injuries can be a diagnostic and therapeutic nightmare, as the knife could potentially have penetrated anything in his left chest (including lung, heart, and/or great vessels) or anything in the abdomen (including colon, small intestine, stomach, spleen, and diaphragm).
Shit.
So I did what I always do in this situation – I put my finger in the hole. Oliver was clearly unhappy with this manoeuvre, but the laceration was quite deep, extending towards his midsection underneath his 12th rib. I could not feel any obvious penetration into his chest or abdomen, but unfortunately knife blades tend to be thinner than my finger, so this is not a perfect test in any way. Since all of his vital signs remained rock stable, his next stop (after a normal chest x-ray) was the CT scanner. Much to my surprise and chagrin, though the scan did not show any injury in the chest, it did show a small amount of fluid (read: blood) in the left upper abdomen along with a few dots of air where they did not belong.
Shit!
While the air could have come from the outside world, it was more likely to be leaking out from a hollow organ (ie stomach, small intestine, or colon). However, not wanting to base my decision solely on a picture on a computer screen, I went back to examine Oliver, whose vital signs were still completely normal (and probably better than mine at that moment). His abdomen was still soft, flat, and completely nontender (except at the stab wound). At this point my options were:
- Patch him up and sent him home, which was a terrible idea.
- Observe him for the next 12 hours to see if any signs of peritonitis develop from a perforation that I conveniently decided to ignore for half a day. This is only a slightly less bad option, because by the time peritonitis develops, Oliver would already be (by definition) sick as hell.
- Take Oliver to the operating room, insert a laparoscope into his abdomen, and take a look around.
Ninety minutes later I had a laparoscope in his abdomen, where I was able to see a small amount of blood in the left upper abdomen as well as a small laceration to his diaphragm.
Wait wait wait Doc, 90 minutes? Why the hell did it take you 90 minutes to get him to theatre? That's malpractice! I'm going to report you etc etc.
Hold on there, bucko. Remember how I said Oliver was my second penetrating trauma of the day? Well the first one came in exactly two minutes before Oliver did. He was much sicker than Oliver was, so I had to take him to theatre first. Remember also when I said he would be addressed in a future post? He will. I just haven't gotten to it yet. So hold onto your stupid report and stick it somewhere dark.
Anyway, the diaphragm laceration certainly needed to be repaired, but I also need to make sure nothing else had a hole in it that needed repair. I remove the laparoscope and opened him up the old fashioned way, but after an exhaustive search the only other injury I found was a very small laceration to his omentum. The air on the CT scan had indeed come from the outside world, but assuming that without doing surgery is a potentially lethal mistake. Fortunately for Oliver this was the best possible outcome – his postoperative course should be short, about two to three days, and hopefully uneventful.
Hopefully. (Foreshadowing . . .)
I heaved a big sigh and repaired his diaphragm, everybody gave each other a high-five for a job well done (not really), and I closed. I went to see Oliver the next morning at 7 AM, and he was putting his clothes on, getting ready to leave. You know, 12 hours after major surgery.
Uh . . .
"Oh hey Doc. Listen, I got to go. I have things I need to do at home," he told me with a small wince of pain as he buttoned his shirt. I looked at him sternly and then very slowly and carefully and using very small words explained to him that he just had major surgery 12 hours earlier, and he should expect to be in the hospital for 2 to 3 more days. But Oliver would have nothing of it.
"Nope, sorry I got things I gotta do at home. I've been walking, I feel fine, I need to go." I heaved a very heavy sigh, looked at him even sternlier (yes, that should totally be a word), and explained everything that I had just explained, this time a bit more slowly, a bit more forcefully, and using even smaller words so that he would be sure to understand.
Nope. The nurse called me an hour later to alert me that he had indeed left the hospital against medical advice.
And then one of the emergency physicians called me seven hours after that to tell me that he was back.
Of course.
When I went in to see him the following morning, he looked only mildly abashed, like he had barely done anything wrong. "Welcome back," I told him with a scowl. "Yeah, I probably shouldn't have left, right?" he said, finally looking up from his mobile.
"Right," I told him in that same stern voice I had used before. "That was a stupid thing to do. Really stupid. I expect you to stay here in hospital this time until I discharge you. Clear?" He simply nodded and went back to playing a game on his mobile.
As expected, Oliver had normal post-laparotomy pain which is best treated, you know, in a hospital. He stayed in hospital for 3 more days until his bowels woke back up (which is normal after major abdominal surgery), and he then went home again.
But not until I discharged him.
Saturday, 9 September 2017
No, Jahi McMath is still not alive
I'm stunned.
I'm simply stunned.
As you can probably imagine, considering everything I see in my trauma bay, it takes a lot to stun me. The most recent judge in the Jahi McMath case managed to do it.
If you aren't familiar with Jahi, you can read more about her sad case here (there are links to other updates in that post). In short, at age 13 she underwent a complicated nasopharyngeal surgery back in December of 2013. The surgery reportedly went well, but postoperatively she bled to the point of cardiac arrest and eventual brain death (which was verified by 6 separate physicians). Her mother fought the diagnosis, and she moved Jahi to New Jersey where she still resides, on a ventilator and unresponsive.
Or is she?
The family has released several videos showing Jahi supposedly moving to verbal cues and another showing her overbreathing her ventilator (if you aren't familiar with that term, just google it). They claim this proves she is not brain dead, and they found a well-known brain death critic named Alan Shewmon, a paediatric neurologist, to supposedly corroborate their hypothesis.
In response to this, judge Stephen Pulido this past week declared that there is a possibility that Jahi is not in fact brain dead, so he has decided to send the case to a jury to decide if Jahi is still dead or if she no longer satisfies the requirement for brain death.
There are several glaring problems, all of which have combined to flabbergast me.
The first and biggest problem I have here is that Alan Shewmon HAS NOT EXAMINED HER. He solely relied on the 49 unsubstantiated videos supplied by Jahi's family to formulate his opinion that Jahi does not meet the criteria for brain death. I've seen several of the videos, and I can definitively tell you that they mean exactly jack shit. For example, one of them shows only Jahi's foot moving in response to her mother's voice. That's it, just her foot. There is no indication how long they were taking video, if she was moving her foot prior to the commands being given, etc. It's absolutely meaningless.
Let me reiterate this in no uncertain terms: Alan Shewmon has averred in a sworn statement given to the court that Jahi no longer meets criteria for brain death based solely on these videos. The only instance when he examined her was in December of 2014, at which time he stated that she was not in any way responsive (see paragraph 9). He has NOT re-examined her since. Not to mention the fact that nothing in the videos is acceptable in either diagnosing or ruling out brain death.
And Judge Pulido not only accepted Shewmon's ridiculous statement, he has kicked this to a jury to decide in response to it.
Since when does a jury get to decide who is living or dead? I thought that was the job of doctors. Has medicine advanced to the point where a group of twelve people can make medical diagnoses? And who the fuck decided it was a good idea to do that based on the testimony of a doctor who hasn't even examined the damned patient?
Consider this - if I were to make a diagnosis on a patient I had not examined, what would you call me? At best, you should call me unethical. At worst, a quack. And even worse, consider this: Judge Pulido is asking a jury, presumably without any medical training whatsoever, to synthesise and assess information that even experts would have difficulty with? Are you fucking kidding me?
This case has officially become a farce. It was sad and risible before, but this latest development is absolutely ludicrously preposterous. I don't know how else to put it.
As I have said many times before, if new evidence comes to light showing that Jahi is in fact not brain dead, I will recant everything I have said and state without question that I was wrong. Until then, this is fucking ridiculous.
I'm simply stunned.
As you can probably imagine, considering everything I see in my trauma bay, it takes a lot to stun me. The most recent judge in the Jahi McMath case managed to do it.
If you aren't familiar with Jahi, you can read more about her sad case here (there are links to other updates in that post). In short, at age 13 she underwent a complicated nasopharyngeal surgery back in December of 2013. The surgery reportedly went well, but postoperatively she bled to the point of cardiac arrest and eventual brain death (which was verified by 6 separate physicians). Her mother fought the diagnosis, and she moved Jahi to New Jersey where she still resides, on a ventilator and unresponsive.
Or is she?
The family has released several videos showing Jahi supposedly moving to verbal cues and another showing her overbreathing her ventilator (if you aren't familiar with that term, just google it). They claim this proves she is not brain dead, and they found a well-known brain death critic named Alan Shewmon, a paediatric neurologist, to supposedly corroborate their hypothesis.
In response to this, judge Stephen Pulido this past week declared that there is a possibility that Jahi is not in fact brain dead, so he has decided to send the case to a jury to decide if Jahi is still dead or if she no longer satisfies the requirement for brain death.
There are several glaring problems, all of which have combined to flabbergast me.
The first and biggest problem I have here is that Alan Shewmon HAS NOT EXAMINED HER. He solely relied on the 49 unsubstantiated videos supplied by Jahi's family to formulate his opinion that Jahi does not meet the criteria for brain death. I've seen several of the videos, and I can definitively tell you that they mean exactly jack shit. For example, one of them shows only Jahi's foot moving in response to her mother's voice. That's it, just her foot. There is no indication how long they were taking video, if she was moving her foot prior to the commands being given, etc. It's absolutely meaningless.
Let me reiterate this in no uncertain terms: Alan Shewmon has averred in a sworn statement given to the court that Jahi no longer meets criteria for brain death based solely on these videos. The only instance when he examined her was in December of 2014, at which time he stated that she was not in any way responsive (see paragraph 9). He has NOT re-examined her since. Not to mention the fact that nothing in the videos is acceptable in either diagnosing or ruling out brain death.
And Judge Pulido not only accepted Shewmon's ridiculous statement, he has kicked this to a jury to decide in response to it.
Since when does a jury get to decide who is living or dead? I thought that was the job of doctors. Has medicine advanced to the point where a group of twelve people can make medical diagnoses? And who the fuck decided it was a good idea to do that based on the testimony of a doctor who hasn't even examined the damned patient?
Consider this - if I were to make a diagnosis on a patient I had not examined, what would you call me? At best, you should call me unethical. At worst, a quack. And even worse, consider this: Judge Pulido is asking a jury, presumably without any medical training whatsoever, to synthesise and assess information that even experts would have difficulty with? Are you fucking kidding me?
This case has officially become a farce. It was sad and risible before, but this latest development is absolutely ludicrously preposterous. I don't know how else to put it.
As I have said many times before, if new evidence comes to light showing that Jahi is in fact not brain dead, I will recant everything I have said and state without question that I was wrong. Until then, this is fucking ridiculous.
Friday, 1 September 2017
Diversity
This probably goes without saying, but the world of trauma is pretty damned diverse. I don't mean to say that trauma is different from other medical specialties in that way, because I'm sure every doctor feels the same way about his or her chosen field. However, all those other doctors are wrong. Trauma is clearly the best.
I kid, I kid. Sort of. Not really.
Think about it though - GPs see mostly elderly people with chronic diseases like hypertension and diabetes and high cholesterol, but also the odd patient with back pain, a sniffle, various other aches and pains, or a vague sense of unease. Not so diverse. Specialists only see patients in their particular chosen area. Trauma, on the other hand, is so varied is because we see every and any manner of traumatic injury, intentional, accidental, and otherwise: car accidents, motorcycle crashes, falls (from standing, off ladders, out of windows, from bed, from pub stools), stabbings, assaults, gunshot victims, bicycle crashes, animal attacks (these stories are usually the best), industrial accidents, sports accidents, and other. Diversity.
I kid, I kid. Sort of. Not really.
Think about it though - GPs see mostly elderly people with chronic diseases like hypertension and diabetes and high cholesterol, but also the odd patient with back pain, a sniffle, various other aches and pains, or a vague sense of unease. Not so diverse. Specialists only see patients in their particular chosen area. Trauma, on the other hand, is so varied is because we see every and any manner of traumatic injury, intentional, accidental, and otherwise: car accidents, motorcycle crashes, falls (from standing, off ladders, out of windows, from bed, from pub stools), stabbings, assaults, gunshot victims, bicycle crashes, animal attacks (these stories are usually the best), industrial accidents, sports accidents, and other. Diversity.
I can't really categorise Mauricio (not his real name™) in any other way, so he must therefore be an other.
If there is one thing I've learned from watching crime shows, it is don't run from the police. Don't run on foot, don't flee in a car, don't speed off on a motorcycle, just don't fucking run. No matter how fast you think you are, even if the officers themselves are not terribly swift, the police dogs and helicopters are faster than you. Mauricio apparently either never watched these shows or isn't smart enough to pick up the message.
My bet is the latter.
The walk-in clinic is an off-shoot of A&E/ED in which I have very little involvement. If you think I avoid the emergency department and their "I just, I don't know, I just don't feel right" patients, you better believe I avoid this part of it. This area is reserved for the non-emergent emergencies (ie the patients who can usually wait to see their GP the following day or week or year), but unfortunately I still get the occasional call from docs there about patients with facial fractures they can't deal with or lacerations they don't want to deal with. The stories are rarely good, which is why I never tell them.
Until Mauricio.
Mauricio had been brought to the walk-in clinic by police after what they called a "fall". They are not medics, so I can't really fault them for not giving an appropriate consultation, but I will anyway because Mauricio was not a fall, as we all found out later. Regardless, the emergency physician's workup on Mauricio included a CT of his brain which found two surprising results: 1) he actually had a brain, and 2) a subdural haematoma, which was why I was called. He was complaining of a headache (obviously) though he was neurologically intact. Despite the rather ugly looking scan, he had no weakness, numbness, or any other complaint. He ultimately would not need surgery, but he still needed to be closely watched in intensive care to make sure that his brain didn't swell and the bleeding didn't worsen.
Despite the two surprises we already had, the diagnosis wasn't the real surprise. It was the mechanism of injury that was.
Mauricio had been caught trying to steal a car. I say trying because he apparently is a shit car thief and could not even get in the door. A bystander apparently saw him using a clothes hanger to try to unlock the door (yes, really) and called the police. When they arrived about 15 minutes later, he still hadn't figured out that 1) the hanger would never work on that particular model car, and 2) a rock would have broken the window and gotten him into the car much more easily. Anyway, when the police told him to freeze (or whatever the hell they actually yell in 2017), he did not freeze. No, he ran.
And ran.
And ran.
Right into a brick wall.
Now last time I checked, brick walls are neither small nor particularly mobile, so surely Mauricio was just so drunk that he stumbled into it, right? Nope. His blood alcohol was negative, as was his urine tox screen. He actually literally just ran into a brick wall.
I can add this to the pile of "Well, I doubt I'll ever see that shit again."
My bet is the latter.
The walk-in clinic is an off-shoot of A&E/ED in which I have very little involvement. If you think I avoid the emergency department and their "I just, I don't know, I just don't feel right" patients, you better believe I avoid this part of it. This area is reserved for the non-emergent emergencies (ie the patients who can usually wait to see their GP the following day or week or year), but unfortunately I still get the occasional call from docs there about patients with facial fractures they can't deal with or lacerations they don't want to deal with. The stories are rarely good, which is why I never tell them.
Until Mauricio.
Mauricio had been brought to the walk-in clinic by police after what they called a "fall". They are not medics, so I can't really fault them for not giving an appropriate consultation, but I will anyway because Mauricio was not a fall, as we all found out later. Regardless, the emergency physician's workup on Mauricio included a CT of his brain which found two surprising results: 1) he actually had a brain, and 2) a subdural haematoma, which was why I was called. He was complaining of a headache (obviously) though he was neurologically intact. Despite the rather ugly looking scan, he had no weakness, numbness, or any other complaint. He ultimately would not need surgery, but he still needed to be closely watched in intensive care to make sure that his brain didn't swell and the bleeding didn't worsen.
Despite the two surprises we already had, the diagnosis wasn't the real surprise. It was the mechanism of injury that was.
Mauricio had been caught trying to steal a car. I say trying because he apparently is a shit car thief and could not even get in the door. A bystander apparently saw him using a clothes hanger to try to unlock the door (yes, really) and called the police. When they arrived about 15 minutes later, he still hadn't figured out that 1) the hanger would never work on that particular model car, and 2) a rock would have broken the window and gotten him into the car much more easily. Anyway, when the police told him to freeze (or whatever the hell they actually yell in 2017), he did not freeze. No, he ran.
And ran.
And ran.
Right into a brick wall.
Now last time I checked, brick walls are neither small nor particularly mobile, so surely Mauricio was just so drunk that he stumbled into it, right? Nope. His blood alcohol was negative, as was his urine tox screen. He actually literally just ran into a brick wall.
I can add this to the pile of "Well, I doubt I'll ever see that shit again."
Subscribe to:
Posts (Atom)
Not dead
I'll start this post by answering a few questions that may or may not be burning in your mind: No, I'm not dead. No, I didn't g...
-
EDIT: New and improved version, now with 83 of your favourite myths. Ooooooh boy. I have no idea what kind of rabbit hole I'm entering...
-
NOTE: If you haven't heard of Jahi McMath's story, you can read about it here . I go into more details here , here , here , and ...
-
I tried my best, I really did. I've seen the article, I read it, and I tried to ignore it. I had fully intended to leave it alone unti...








